Advanced bone graft materials play an active role in the bone healing process by positively influencing cellular healing.
Biogennix, October 5, 2022 – OrthoSpineNews – Featured Article
Synthetic bone graft products first became available to surgeons in the early 1990s. Many of the initial products were based on porous calcium phosphate materials and were clinically effective. However, they solely functioned as an osteoconductive scaffold that supported bone growth on the surface of the material. As a result, these first-generation products played a passive role in bone formation and were not actively involved in the cellular healing process. Recent innovations in the synthetic bone graft field have resulted in next-generation materials that now have the ability to positively influence the cellular bone formation response.
Today, advanced synthetic products have been specifically engineered with unique properties that allow the material to play an active role in bone formation. The potential healing benefits of advanced synthetics are leading a growing number of surgeons to choose these innovative products over conventional bone graft options.
To demonstrate the value of advanced bone grafts, we will compare them to first-generation graft materials. By examining how these two types of bone grafts differ in material properties, we can see why advanced synthetic products are gaining favor in the evolving bone graft market.
Passive vs. Active: The Difference Between Two Types of Bone Grafts
There are a variety of bone graft products on the market that have different compositions, structures, and forms. Characterizing bone grafts by their involvement in the healing process results in two types of bone grafts:
- Passive Bone Grafts: Bone graft materials that are solely osteoconductive (i.e. only function as a scaffold for bone formation); typically associated with first-generation synthetics.
- Active Bone Grafts: Bone graft materials that are osteoconductive, but also have the ability to positively influence the cellular bone formation process; typically associated with advanced synthetics like Biogennix TrelCor®products, advanced demineralized bone matrix (DBM) products containing enhanced bone derived carrier technology, growth factors, and Bioglass.
Passive Bone Grafts
The role of a passive bone graft in the healing process is to function as a scaffold for bone formation. These materials are typically porous and allow bone formation on the material’s surface and through its porosity. The graft resorbs over time and eventually is fully replaced by bone.
Products in this category have been used for years with clinically successful outcomes. However, due to their limited role in the bone regeneration process, passive bone graft products may take longer to fully fill with new bone, or may result in a reduced bone formation response in challenging bone grafting applications, such as large voids or patients with multiple comorbidities.
Active Bone Grafts
The limitations of passive grafts can be overcome with the use of products based on bone graft materials actively involved in the bone healing process. Bone graft materials are considered biologically active when they can promote or enhance the cellular regeneration process.
This can be accomplished through multiple mechanisms of action. For example, a growth factor product that contains bone morphogenetic protein (specifically BMP-2) has been shown to increase osteoblast proliferation and function and promote stem cell differentiation due to the interaction of the BMP protein with bone forming cells. Bioglass products accomplish the same cellular effect, but through a different mechanism. Once implanted, Bioglass undergoes a slow dissolution process that releases ions that stimulate the surrounding cells.
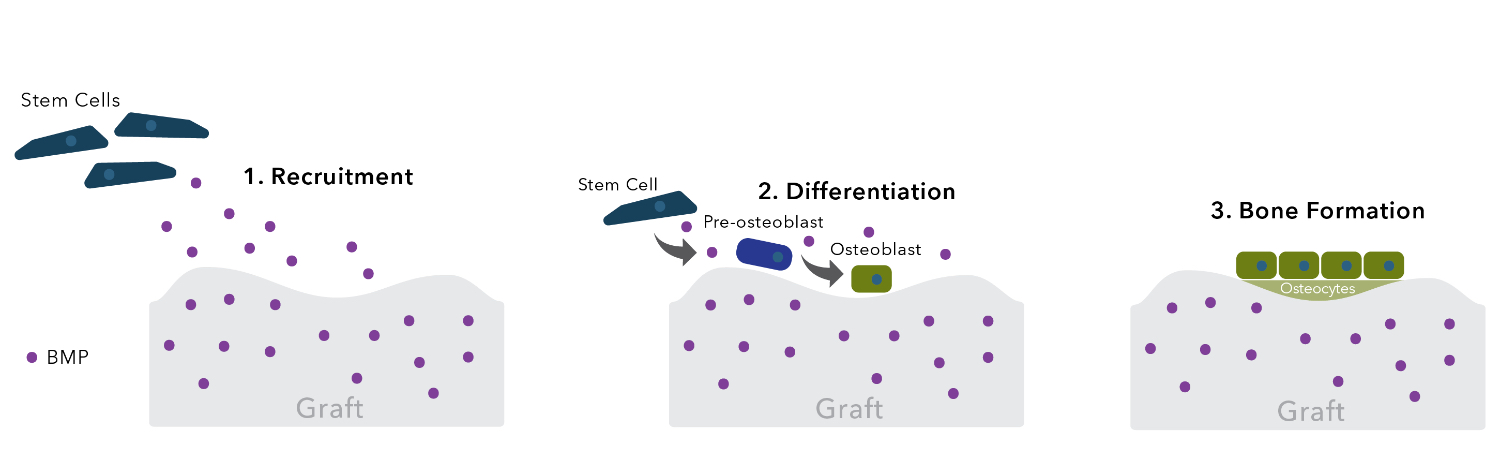
Growth factor based bone grafts play an active role in bone healing through protein-based cell stimulation.
Next-Generation Technology Is Transforming the Synthetic Bone Graft Market
The introduction of biologically active bone graft materials into the synthetic graft market provides surgeons with products based on newer and more advanced technologies. Next-generation synthetic materials play an active role in bone regeneration by incorporating two advanced concepts: precisely controlling the material’s surface structure and surface composition.
Surface Morphology
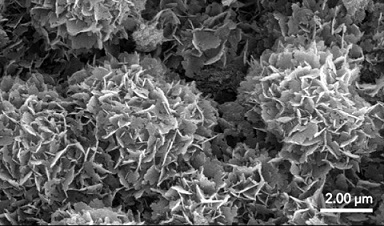
Surface morphology describes the size, shape, and structure of a material’s surface. Multiple studies have shown that materials with nanosized surface features can positively influence bone formation (Zhang 2017; Duan 2018). Osteoblasts that attach to nanosurfaces will show increased proliferation and cell function. Further, nanostructured surfaces have been shown to cause the differentiation of stem cells into osteoblasts. Bone graft materials that incorporate a nanocrystalline region on the entire surface of a material can lead to enhanced bone formation as compared to first-generation grafts that feature smooth surfaces.
Material Composition
The core property of all bone graft materials is the ability to support bone formation directly on the surface of the material. The bone formation process is based on a cellular response that includes osteoblasts, osteoclasts, and stem cells. The first synthetic bone graft products introduced to the market were generally based on the calcium phosphate component of bone mineral. However, bone mineral is not a pure calcium phosphate material that is commonly found in first generation synthetic products, such as hydroxyapatite (HA) or tricalcium phosphate (TCP). Bone mineral consists of a substituted form of calcium phosphate that includes carbonate and other elements such as magnesium, zinc, and iron.
Recently, researchers have found that subtle differences in the surface composition of calcium phosphate bone graft materials can have a significant effect on the bone formation process (Spence 2006; Hyashi 2019). The surface composition affects the degree and duration of the initial cellular preparation phase that occurs prior to bone formation.
Carbonated apatite materials such as hydroxycarbanoapatite (HCA) can have an accelerating effect on the healing process. This is attributed to the presence of carbonate substitution within HCA, which makes it biomimetically similar to natural bone mineral. Due to this similarity, the initial cellular preparation phase of HCA is significantly shortened, and the bone formation response occurs sooner than with first-generation forms of calcium phosphate.
Experience the Benefits of Advanced Synthetic Bone Grafts
Advancements in synthetic bone graft materials have resulted in next-generation bone graft products that are actively involved in the bone formation process. These advanced bone graft materials represent an improvement over passive bone graft materials that are based on first-generation technology. Advanced synthetics have the potential to produce better patient outcomes than their predecessors, as they offer regeneration-influencing surface morphology and composition. Advanced synthetic materials represent the future of bone graft technology and are rapidly being adopted by surgeons.
Biogennix TrelCor advanced bone graft solutions combine nanocrystalline HCA surface technology with a biomimetic pore architecture that can improve clinical outcomes. Multiple studies have shown that nanocrystalline surface morphology can positively influence cell attachment and differentiation, while an HCA surface composition can encourage healing to begin sooner compared to HA or TCP. Contact our team to learn more about the types of bone grafts we offer and the clinical benefits of Biogennix technology.
As a recognized leader in advanced bone graft technologies, Biogennix is committed to bringing high-quality educational content to our field. The Biogennix Blog covers technical topics ranging from basic bone graft science to advanced osteobiologic principles. The Blog also discusses market trends and industry challenges. We thank you for reading and invite you to learn more about us here.
Contact: info@biogennix.com