–Study to Evaluate Safety and Tolerability of Simultaneous Implant of Spinal Fusion and Neuromodulation Devices in Chronic Lower Back Pain Patients
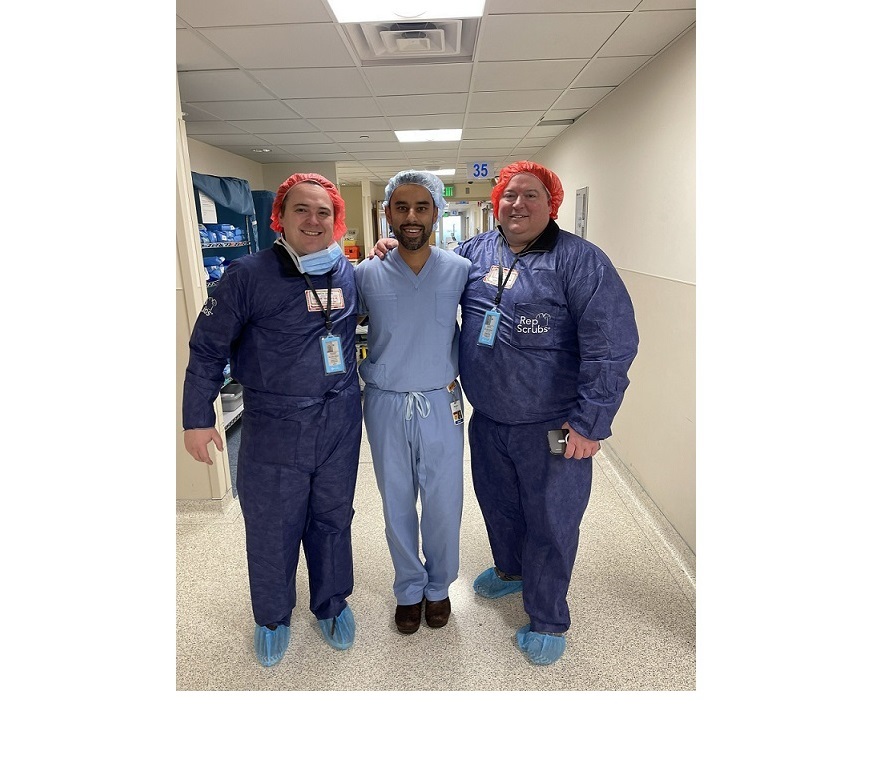
EDEN PRAIRIE, Minn., Jan. 9, 2023 /PRNewswire/ — Justin Zenanko, CEO of SynerFuse, Inc., a Minnesota-based medical device company, is pleased to announce that for the first time in the world, a solo spine surgeon performed the groundbreaking SynerFuse procedure. Rohan Lall, MD, at once both performed a spinal fixation procedure and implanted a neurostimulator with leads on the eighth patient in the company’s proof-of-concept study.
“So far in the study, the SynerFuse procedure has been efficient and straightforward to perform,” said Lall. “The industry has seen the efficacy of DRG stimulation for patients with chronic pain, and it is very exciting to be able to study incorporating it earlier in the treatment process for these patients in an attempt to reduce their pain levels and needs for opioids. I believe this will become widely adopted in spine surgery.”
The SynerFuse proof-of-concept study involves combining spinal fusion with the implant of a neurostimulator to provide stimulation of the dorsal root ganglion (DRG), a key nerve structure along the spine that can be targeted with neuromodulation to treat chronic neuropathic pain, to provide relief to patients suffering from chronic lower back pain (cLBP). Patients undergoing an initial spinal fusion, among other criteria, are eligible for the study. The SynerFuse proof-of-concept study supports the enrollment of up to 20 patients.
“This is an important step toward demonstrating that our combined procedure can be performed without needing two surgeons,” said Zenanko. “Spinal fixation procedures today are performed by one spine surgeon. This study aims to conclude that one spine surgeon can also perform the integrated SynerFuse procedure. This is an important step toward adoption of the procedure.”
“The implantation of the eighth patient in our proof-of-concept study is an important milestone for SynerFuse,” said Zenanko. “With each new patient, we’re one step closer to demonstrating the viability of our non-narcotic concept for spinal fusion patients with chronic lower back pain.”
“Bringing this patient-focused therapy from concept to the eighth implant is a true testament to collaboration within our company and with our surgeon and staff partners at the University of Minnesota Medical School and M Health Fairview University of Minnesota Medical Center,” said Molnar.
Seven patients previously had a neurostimulator with leads implanted by Michael C. Park, MD, PhD, and spinal fixation by Rohan Lall, MD, and Jonathon Sembrano, MD, at M Health Fairview University of M Health Fairview University of Minnesota Medical Center.
More information about SynerFuse is available at www.synerfuse.com.
About Chronic Lower Back Pain (cLBP)
cLBP is defined as lower back pain that continues for 12 weeks or longer, even after an initial injury or underlying cause of acute lower back pain has been treated.1 With more than 500,000 procedures performed annually, spinal fusion remains a common treatment for spinal instability, albeit with a high incidence of residual neuropathic pain2. Up to 40% of patients who undergo spinal fusion end up with Failed Back Surgery Syndrome (FBSS), a condition resulting in significant, lingering neuropathic pain, costing the U.S. healthcare system $20B per year and significantly affecting the quality of life of patients3.
About SynerFuse
SynerFuse is a Delaware corporation based in Minnesota—the heart of Medical Alley and the cradle of neuromodulation and medical device innovation. SynerFuse believes that individuals with cLBP/FBSS and their providers deserve an alternative option than spinal fusion alone. Even when spinal fusion is successful, it can often result in residual chronic neuropathic pain and use of addictive opioids. The company is working to create a non-narcotic pain management for chronic low back pain with a patented therapy that integrates spinal fusion hardware and an active neuromodulation system. For more information on the company, please visit www.synerfuse.com.
This communication contains information about an investigational product. This product is limited by Federal (U.S.) law to investigational use only. SynerFuse makes no claims regarding the safety or effectiveness of the unapproved investigational product. The intent of providing this information is to convey research and development initiatives underway at SynerFuse.
1 See “Low Back Pain Fact Sheet.” National Institute of Neurological Disorders and Stroke, https://www.ninds.nih.gov/low-back-pain-fact-sheet#:~:text=Chronic%20back%20pain%20is%20defined, back%20pain%20has%20been%20treated, accessed October 17, 2022.
2 Karen L. Saban et al., “Health-Related Quality of Life of Patients Following Selected Types of Lumbar Spinal Surgery: A Pilot Study,” Health and Quality of Life Outcomes 5 (2007), https://doi.org/10.1186/1477-7525-5-71.
3 Farber SH, Han JL, Elsamadicy AA, Hussaini Q, Yang S, Pagadala P, Parente B, Xie J, Lad SP. Long-term Cost Utility of Spinal Cord Stimulation in Patients with Failed Back Surgery Syndrome. Pain Physician. 2017 Sep;20(6):E797-E805. PMID: 28934786; PMCID: PMC8358894.
SOURCE SynerFuse