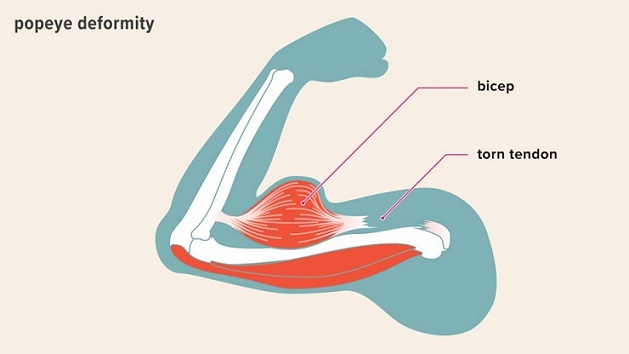
ROSEMONT, Ill., April 26, 2021 /PRNewswire/ — Musculoskeletal injuries comprise a large percentage of hospital admissions for adults1 and often lead to chronic pain and long-term disability. A new review article published in the Journal of the American Academy of Orthopaedic Surgeons® (JAAOS®) recognizes the intimate connection between patients who sustain traumatic orthopaedic injuries and their subsequent psychological effects. The results suggest opportunity to improve overall patient health by attending to psychological and social concerns, along with physical health.

“This review article looks at the majority of recent literature as it pertains to different psychological conditions and how they affect musculoskeletal trauma patients,” said article author Matthew Ciminero, MD. “We sought to demonstrate that of the vast number of people who will undergo orthopaedic trauma in their lifetime, an alarming percentage will develop some form of psychological condition that will ultimately impair daily function.”
Dr. Ciminero was inspired by an upbringing from two parents with Ph.D.s in Psychology and his undergraduate degree in Psychology to investigate the limited referrals to mental health professionals from orthopaedic surgeons treating patients of both elective and traumatic injuries. He teamed up with fellow orthopaedic surgeons from Denver Health, as well as his colleagues at Maimonides Medical Center in Brooklyn, N.Y., to discuss the role of psychological evaluations and the need for improvements in community awareness of post-traumatic injury effects.
The study discovered:
- In patients who had sustained a severe lower limb injury, nearly half were positive for a psychological condition three months later and 42% were positive at two years.
- Early in their treatment, only 12% of patients stated that they used any mental health services and by 24 months, this number only increased to 22%2.
The study also found that by the age of 50 years, 53.2% of women and 20.7% of men will have sustained some form of fracture.3 Soon after sustaining a fracture, psychological factors can predict pain and disability many months after injury, even after controlling for injury severity. Seeing this, the research team also looked to the Major Extremity Trauma Research Consortium (METRC) from 2018, which identified four groups of clinically relevant patients and assessed their risk factors as they pertained to psychological effects after orthopaedic trauma.
“These four groups were low risk/low protection, low risk/high protection, high risk/high protection, high risk/low protection,” Dr. Ciminero said. “Naturally, the high risk/low protection group has a higher chance of experiencing a psychological burden, and thus should be targeted early in their post-operative care to be referred to the appropriate mental health professional.” Risk factors identified by the METRC study included: pain, depression, alcohol and tobacco abuse, and PTSD, while protective factors included: resilience, self-efficacy and social support.
“At six weeks post-injury, a number of patients in the most at-risk cohort had Short Musculoskeletal Function Assessment (SMFA) scores that exceeded disability thresholds, and at one year post-injury, over 90% of that cohort showed similar scores,” Dr. Ciminero said. “In that cohort as well, three quarters of those patients tested positive for depression and PTSD.”
Enlightened by that study, Dr. Ciminero and his co-authors developed a flow chart, as well as gathered screening tools and surveys to aid orthopaedic surgeons in determining at what stage their patients need psychological interventions such as Cognitive Behavioral Therapy (CBT), mindfulness training or other types of mindset training.
The flow chart, presented in the review article, suggests using empathic, verbal inquiries and administering a brief psychological inventory to assess orthopaedic trauma patients for anxiety, depression, PTSD and/or pain. If those tests results are positive, the chart guides physicians towards referring their patients to a mental health professional.
“Our review article offers tools that could be used in both in-patient or office settings, so if a patient is displaying signs of anxiety, depression, PTSD, having difficulty rehabilitating or experiencing pain-control issues, they can quickly and effectively be referred to mental health professionals,” Dr. Ciminero said.
In the search for the best available treatment for orthopaedic trauma patients, Dr. Ciminero has found CBT to be highly effective. He noted, “Despite the stigma of mental health treatment in our society, studies show there is a high patient compliance rate when offered psychological interventions. In one study, we saw a decrease in anxiety and depression (16% and 66% respectively) among geriatric patients with hip fractures who were given psychotherapy for 45 minutes twice a week.”
Moving forward, Dr. Ciminero plans to continue to pursue this topic further. He posits a possible multi-center randomized controlled trial of level-1 trauma patients, categorized by either traumatic location or injury severity, who are then treated with either the standard post-operative rehab and pain management, CBT, or CBT combined with Selective Serotonin Reuptake Inhibitors (SSRI).
“We are always looking for answers to what we can do to improve outcomes and care for our patients the best way possible,” Dr. Ciminero said.
To schedule an interview about this JAAOS® review article, email media@aaos.org. For information about AAOS’ Appropriate Use Criteria (AUC) for the evaluation of psychosocial factors influencing recovery from adult orthopaedic trauma, visit the OrthoGuidelines website and free mobile app.
More information about the AAOS
Follow the AAOS on Facebook, Twitter, LinkedIn and Instagram.
1 Vranceanu AM, Hageman M, Strooker J, Ter Meulen D, Vrahas M, Ring D: A preliminary RCT of a mind body skills-based intervention addressing mood and coping strategies in patients with acute orthopaedic trauma. Injury 2015;46:552-557.
2 McCarthy ML, MacKenzie EJ, Edwin D, Bosse MJ, Castillo RC, Starr A: Psychological distress associated with severe lower-limb injury. J Bone Joint Surg Am 2003;85-A:1689-1697.
3 Busse JW, Heels-Ansdell D, Makosso-Kallyth, et al: Patient coping and expectations predict recovery after major orthopaedic trauma. Br J Anaesth 2019;122:51-59.
SOURCE American Academy of Orthopaedic Surgeons