Elizabeth Hofheinz, M.P.H., M.Ed.
“Grandpa fractured his hip” doesn’t have to be a death sentence.
In a first-of-its-kind study, researchers from Texas have determined that walking a mere 5 feet (or more) after hip fracture surgery can lower the chances of postop complications. Their study, “Walking Greater Than 5 Feet After Hip Fracture Surgery Is Associated With Fewer Complications, Including Death,” was published in the March 1, 2021 edition of the Journal of the American Academy of Orthopaedic Surgeons.
At the time of the study, co-author Richard VanTienderen, D.O. was a resident with the Foster School of Medicine’s orthopaedic surgery program at the Texas Tech University Health Sciences Center (TTUHSC) El Paso and William Beaumont Army Medical Center. Dr. VanTienderen told OSN, “Placing a physical therapy consult for assistance with post-operative mobilization is routine in the aftercare of patients being treated surgically for a geriatric hip fracture. The orthopaedic team at TTUHSC El Paso would regularly encourage patients to attempt to ambulate early in the post-operative course and discuss their ambulatory status during morning report and while rounding.”
“While following the clinical course of these patients, I began to notice a trend that it seemed as though patients who refused to ambulate early on were having longer hospital lengths of stay as well as increased morbidity and mortality. Based on this observation I began a search to see if there was literature that supported this. Finding none, I proposed the idea to perform a retrospective study to test my hypothesis that early ambulation after hip fracture surgery is associated with decreased post-operative morbidity and mortality.”
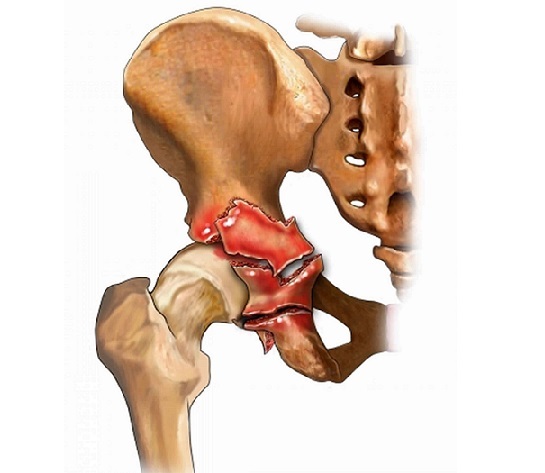
So he and several colleagues performed a retrospective review on 163 patients with hip fractures from October 2015 through September 2017 (64 femoral neck, 88 intertrochanteric, and 11 subtrochanteric fractures). All ambulatory patients at least 65 years old, with a low-energy fracture, and who underwent surgical treatment were included. Physical therapy notes were used to track postoperative ambulation, and medical records were reviewed for 90-day postoperative complications.
Minor effort, big payoffs
“Results from this study suggest a distance and timing threshold associated with more successful postoperative outcomes after hip fracture fixation,” stated Dr. VanTienderen to OSN. “Patients that met inclusion criteria for this study were separated into an ambulatory cohort (those that were able to walk greater than five feet within 72 hours of surgery) and a nonambulatory cohort (those that were unable to walk greater than five feet within 72 hours of surgery). Specifically, the nonambulatory cohort had an increased overall complication rate (77% versus 31%), as well as higher incidence of myocardial infarction, pneumonia, ICU admission, deep vein thrombosis, cardiac arrest, sepsis, and death or hospice transfer. The ambulatory cohort also had decreased hospital length of stay.”
“To our knowledge, this is the first study that specifically discusses outcomes after geriatric hip fracture surgery associated with a post-operative mobilization timeframe and ambulation distance. Knowledge of these results can help all members of the multidisciplinary team involved in the care of geriatric patients being treated for a hip fracture to inform their patients of the importance of ambulating early after hip fracture surgery and provide motivation for patients to increase their activity levels early on in the rehabilitation process.”
Several directions for future research
“As this article is a single study at a single institution, similar studies performed at other institutions could help validate the results and increase the patient sample size. While a randomized or blinded study is likely not possible for this particular situation, collecting data prospectively would increase the quality and uniformity of the data. Also, as we reported only short-term outcomes, further research could look into if the results of this study are valid for long-term outcomes.”