Elizabeth Hofheinz, M.P.H., M.Ed.
In a cost containment study, four orthopedic trauma surgeons used high-value external fixation implants from the Orthopaedic Implant Company (OIC) that were biomechanically shown to be equivalent to conventional implant company products.
The research, “The Clinical and Economic Impact of High Value External Fixation Utilization at a Level II Trauma Center,” appears in the January 21, 2021 edition of the Journal of Orthopaedic Experience and Innovation.
Regarding the transition of trauma to OP setting, OIC’s President and CEO Itai Nemovicher told OSN, “The landscape has shifted. Medicare and Medicaid are making adjustments to their reimbursement rates as we speak, rewarding more value-driven initiatives that still bring high quality surgical outcomes, which is especially important as more underinsured and uninsured patients are treated in outpatient settings and taking on the costs of their own care out-of-pocket. The financial decisions that surgeons and facilities make regarding orthopaedic implants are going to more frequently have a direct impact on their patients, so it’s imperative that value-based devices become a priority for surgery centers moving forward.”
When OSN asked Nemovicher when he began predicting this, he commented, “As advancements in implant technology and in treatment techniques have been made steadily over the last five to seven years, what we were seeing was that the most high-volume ortho trauma injuries – ankle, wrist, hip, and clavicle – were trickling into outpatient centers at increasing rates from one year to the next, so the full transition that we’re now witnessing was inevitable in a lot of ways.”
“And at the rate this transition is currently progressing, the most likely scenario is that 80% of all orthopaedics, including the majority of trauma, will eventually end up in the outpatient setting, leaving the hospitals with only tumors, Level 1 traumas, complex spine cases, and infections. This is part of the reason we’ve been at the forefront of championing and executing value-based models for pricing and delivery on every single one of our implants – it’s just better for people and it’s better for healthcare.”
Details
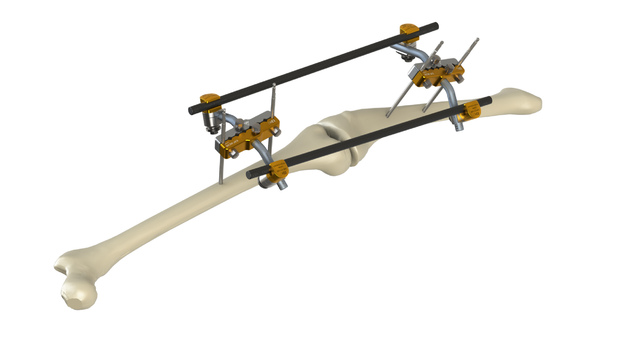
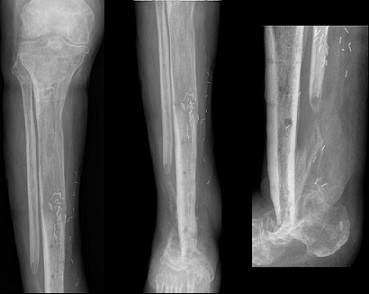
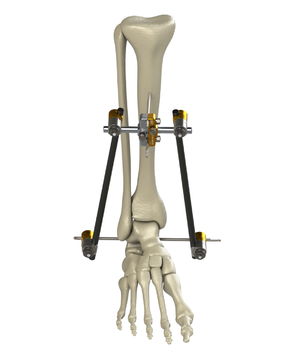
A total of 62 patients with tibial plateau and pilon fractures were treated with the OIC fixation devices and compared to 62 patients treated with conventional brand external fixation devices. The researchers assessed differences in intraoperative and post-operative outcomes in order to determine the clinical efficacy of the high value devices. The team also gathered information from operative records, including intraoperative complications, operative time and estimated blood loss. Any infection, malunion, nonunion or need for repeat surgery were recorded.
The researchers said they found “no significant differences in age, sex, presence of diabetes, smoking or fracture type between the high value and conventional groups. No difference in operative time was noted. No intraoperative or postoperative complications occurred in either group from the time of external fixation to the time of external fixator removal and conversion to definitive fixation. Overall, the hospital realized a 58% reduction in implant costs, an average of $2,200 savings per case and a total savings of $136,400 during the study period.”
OSN asked study co-author David Swanson, M.D. of the Reno Orthopedic Clinic, how they selected the OIC implants. He stated: “High quality, cost-conscious care should be the goal of every provider. Money saved on implants and surgical costs directly benefits both patients and hospitals and surgery centers. We were aware of previous studies involving OIC’s high value instrumentation and frag plates, which yielded substantial cost savings – in some cases as much as 70% in comparison to brand name devices – while maintaining equivalent clinical outcomes.”
“External fixation is one of the most expensive products in orthopaedic trauma and is usually only used for a few days to a few weeks; we wanted to find out if the same kind of cost-effectiveness and clinical equivalency could be demonstrated using OIC’s external fixation system that was seen in their small frag studies.”
“There is an inaccurate perception of high value implants out there as being lesser quality, but the truth is that we confirmed biomechanical equivalence between the high value system and the conventional systems before we even began the study. They met the same FDA standards. And when it was all said and done, the high value external fixation system demonstrated equivalence with brand name systems across all operative, postoperative, and radiographic parameters too. High value implants are not a lesser quality option.”
“Also, in the world of ballooning healthcare costs, we have a responsibility to be cost-conscious for both our patients and our facilities now more than ever. The bottom line is simple: With high value implants, orthopaedic traumatologists have an opportunity to impact the economics of the healthcare cost crisis in a massive, positive way without sacrificing quality of treatment or patient safety.”